Where Is Therapy Going? The Great Split of Mental Health in the Age of Trauma, AI, and Digital Care
Where is therapy going? Discover the future of psychotherapy, from the decline of analysis to the rise of AI chatbots, psychedelics, and somatic experiencing.

Something is happening in therapy. I see it in the way clients talk. In the way therapists now introduce themselves. In how many people from adjacent industries like technology, teaching and HR are now deeply interested in the art of knowing yourselves. I see fewer therapists say "I'm a CBT practitioner." More "I'm trauma-informed." More "somatic." More "nervous system." But this isn't a revolution. It's something more akin to a split.
Since the pandemic, demand for mental health care has surged in both the UK and the US. In early 2021, the CDC reported that 41% of US adults were experiencing symptoms of anxiety or depression - up from 11% in 2019. In England, NHS Digital recorded 4.46 million referrals to NHS Talking Therapies in 2022-23, the highest on record. At the same time, both countries face ongoing workforce shortages in mental health provision.
Normally what happens when demand overwhelms supply, systems adapt. They standardise. They find ways to scale. In England, the vast majority of NHS Talking Therapies remain CBT-based, in line with NICE guidelines. Short-term, goal based therapy is how most people experience therapy.
In the US, meanwhile, digital platforms and app-based interventions have expanded rapidly to fill the void. Venture capital investment has surged - some $2.7 billion was invested in mental health companies last year, as has Silicon Valley's interest in "disrupting" how we heal. But something else has been growing too. What we think therapy "is", has changed.
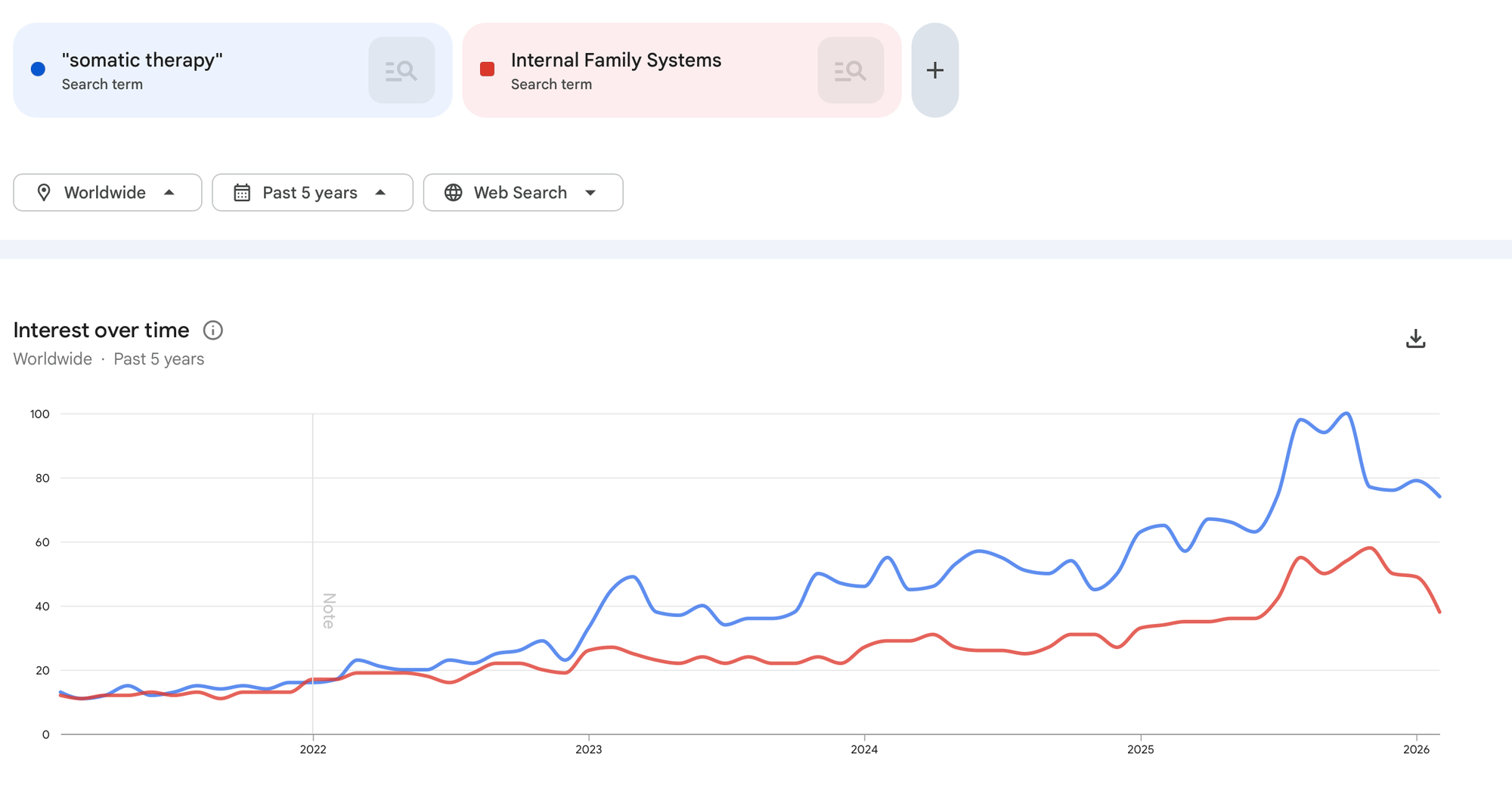
Search interest in terms like "somatic therapy" and "Internal Family Systems" has climbed steadily over the past five years. Trauma has moved from specialist diagnosis to cultural language. Clients arrive already fluent in terms like "regulation" and "attachment wound."
In my own practice, I've noticed a subtle shift. Fewer clients asking simply to reduce symptoms. More asking why their body still reacts long after they understand the thought. Which has led me to ask: where is therapy going? Not only as a practice, but as a cultural phenomenon? As more industries eye up our minds - and its cost to the world economy, which is estimated to reach $6 trillion by 2030 - two distinct camps are emerging.
One direction optimises for scale. The other for depth. And the question shaping the future of mental health may not be which works better - but who gets which.
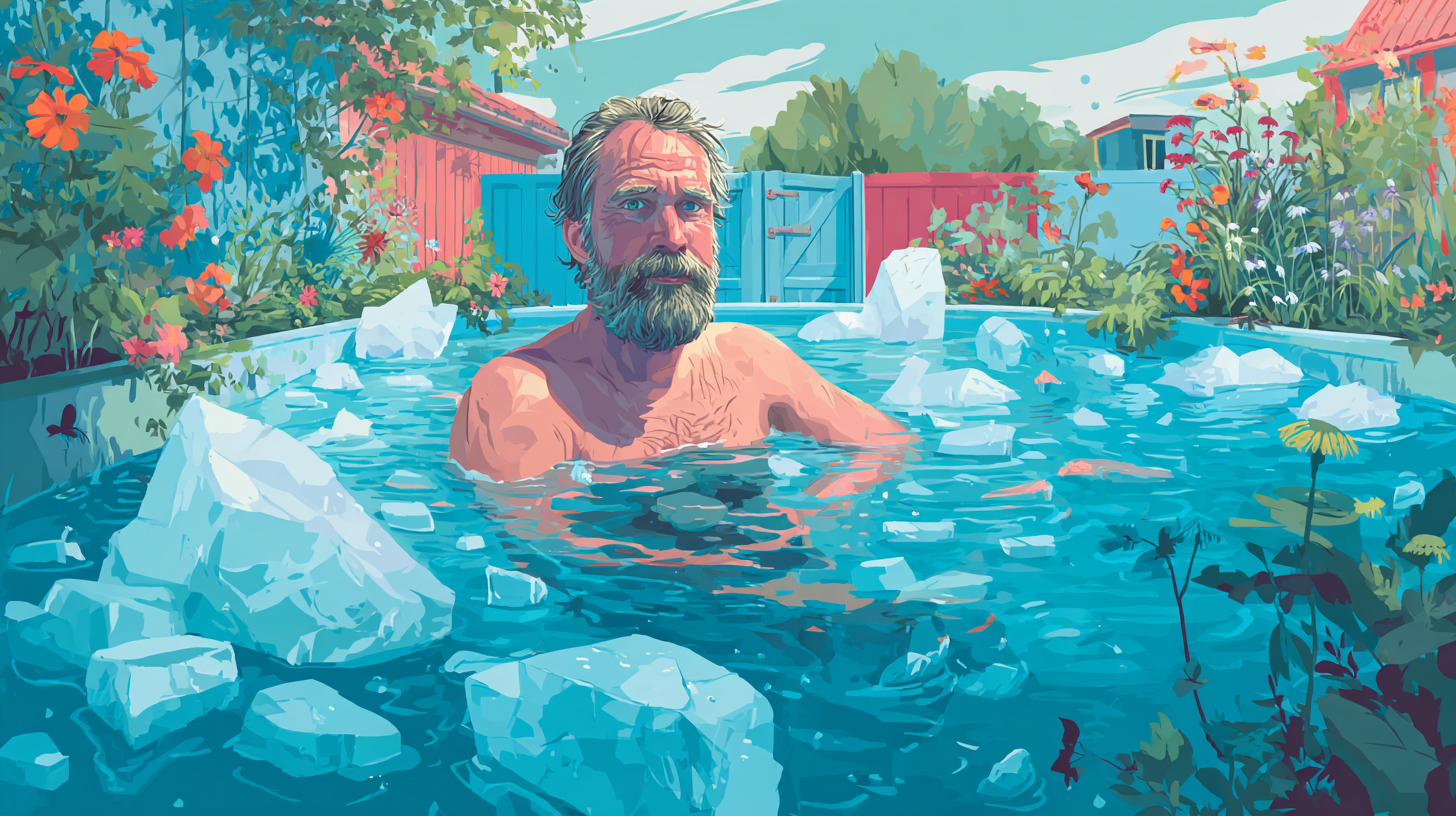
What Is Growing: The Shift Toward Somatic Experiencing and Trauma Therapy

For decades, the institutional centre of gravity in mental health has been cognitive and protocol-driven. Manuals. Worksheets. Measurable outcomes. It has helped millions of people. And yet culturally? The center of gravity is drifting somewhere else. Toward the body.
I feel it in the therapy room. Clients are less interested in arguing with their thoughts and more curious about why their chest tightens before they speak. Why their jaw locks in conflict. Why their body feels older than their years.
And the data suggests this isn't just anecdotal. In the late 1990s, the landmark Adverse Childhood Experiences (ACE) Study found that nearly two-thirds of participants reported at least one adverse childhood experience. More than one in five reported three or more.

Higher ACE scores were strongly associated with increased risk of depression, substance use, heart disease, and suicide attempts. The implications were seismic: trauma was not rare. It was common. And it was biologically consequential.
Subsequent data reinforced this picture. The US National Comorbidity Survey Replication estimated lifetime PTSD prevalence at approximately 6.8% among adults-yet exposure to traumatic events is far higher than formal PTSD diagnoses suggest. In the UK, the Adult Psychiatric Morbidity Survey similarly shows significant trauma exposure across the population, with PTSD more prevalent among women and younger adults.
In other words, trauma isn't a niche clinical concern. It's a public health reality. And increasingly, people know that about themselves.
When Trauma Became Dinner-Table Language

Trauma has been on its own journey. From wars and extreme human experiences to a word that shapes how we heal.

Much of this cultural shift can be traced to the impact of Bessel van der Kolk's The Body Keeps the Score (2014). Whatever one thinks of its theoretical framing, its cultural reach is undeniable. It has spent years on bestseller lists and sold millions of copies globally.
Trauma moved from DSM language into dinner-table language. Around the same time, therapies that explicitly centre trauma and the body began moving from fringe to mainstream.
- Somatic Experiencing, developed by Peter Levine, expanded internationally.
- Internal Family Systems (IFS), created by Richard Schwartz, gained visibility-particularly after being listed as an evidence-based practice for certain populations by the US Substance Abuse and Mental Health Services Administration (SAMHSA).
Meanwhile, EMDR-once controversial-has become firmly established. It is recommended by both the American Psychological Association and the UK's NICE guidelines for PTSD as an evidence-based treatment. This isn't a rejection of cognitive therapy. It's an expansion beyond it. But the expansion is meaningful.
From “Change Your Thoughts” to “Regulate Your Nervous System”

Cognitive Behavioral Therapy (CBT) remains highly effective for many anxiety and mood disorders. It is still the backbone of NHS Talking Therapies. Its evidence base is robust. But something else is happening alongside it.
Clients increasingly arrive already fluent in the language of nervous system regulation. They ask about attachment. About parts. About fight-or-flight. They don’t just want to dispute distorted thoughts—they want to understand why their body reacts before their mind can catch up.
There’s a different assumption underneath this curiosity: that trauma isn’t stored only as story, but as physiology. And that healing might require more than insight. If you zoom out even further, the same gravitational pull shows up in psychedelic-assisted therapy.
Psychedelic Therapies are finding their feet

After decades of prohibition, research has cautiously re-emerged in controlled clinical contexts. In 2023, results published in Nature Medicine found that 71% of participants receiving MDMA-assisted therapy for PTSD no longer met diagnostic criteria at the end of the study, compared to 48% in the placebo-with-therapy group. The FDA granted MDMA-assisted therapy Breakthrough Therapy designation, though regulatory approval remains under review and access is currently limited to clinical research settings.
Psilocybin has also shown promise. A 2021 study published in the New England Journal of Medicine compared psilocybin to escitalopram for depression and found meaningful reductions in depressive symptoms in the psilocybin group.
We should be careful here. These are structured, clinical trials with extensive therapeutic support-not a blanket endorsement of psychedelics. Long-term outcomes are still being studied. Access is tightly controlled. But culturally and scientifically, the direction of travel is clear. Interest is growing in therapies that work through experience-not only cognition.
Two Parallel Ecosystems

When I zoom out, what I see isn’t a revolution. It’s a bifurcation. On one side: short-term, structured, symptom-focused therapy. Often publicly funded. Designed for accessibility and scalability. Optimized for measurable reduction in anxiety and depression.
On the other: longer-term, often privately funded work focused on trauma, attachment, parts, and nervous system repair. Less about worksheets. More about felt experience. Both are responding to real suffering. But they’re built on slightly different assumptions about what that suffering is.
One assumes maladaptive thought patterns are the primary driver. The other assumes unresolved physiological survival responses are.

Neither is inherently wrong. But the cultural momentum-judging by bestseller lists, training enrolments suggests growing public interest in the latter. And maybe that makes sense.
If trauma is common. If it shapes not just what we think, but how our bodies learn to survive. If it's stored not only in memory, but in muscle tension, startle responses, and relational patterns. Then perhaps healing can't live solely in cognition.
What Is in Decline: The End of the "Blank Slate" Therapist

If something is growing in therapy, something else is quietly thinning out. Not collapsing. Not vanishing. But losing its unquestioned authority.
For much of the 20th century, the therapist was trained to be neutral. Contained. A reflective surface. Freud called it the "blank slate." Later traditions softened the language but kept the posture: minimal self-disclosure, carefully managed affect, interpretation over participation.
The idea was immortalised in countless films and TV shows: the therapist as observer. The patient as subject. That stance made sense in its historical context. Traditional psychoanalysis dominated early psychotherapy training in both the US and UK, particularly through the mid-1900s. But training, enrolments and practitioners listing this as a core modality has been in steep decline.
Something has shifted. Clients no longer approach therapy as passive recipients of expert interpretation. They arrive informed. Sometimes over-informed. They have read van der Kolk. They have watched attachment explainers on YouTube. They know the word "gaslighting." They have opinions about trauma. And they are less impressed by emotional distance.

Research over the past three decades has consistently highlighted the importance of the therapeutic alliance as one of the strongest predictors of outcome across modalities. A major meta-analysis found that alliance accounts for a significant proportion of treatment variance, regardless of theoretical orientation. In other words, the relationship matters at least as much as the technique.
That finding has quietly undermined the supremacy of stance-based authority. Even within CBT there has been evolution. Third-wave approaches such as Acceptance and Commitment Therapy (ACT) and Compassion-Focused Therapy (CFT) explicitly incorporate mindfulness, self-compassion, and emotional processing. Schema Therapy integrates attachment theory and experiential techniques. The field has not stood still.
But outside public systems, the appetite for purely protocol-driven therapy appears to be softening.
In England, NHS Talking Therapies remain overwhelmingly CBT-based, and recovery rates hover around 50% according to NHS Digital's 2022-23 report. That is not failure. It is meaningful impact at scale. But it also means roughly half of people completing treatment do not meet recovery criteria.
In the US, similar critiques have emerged about brief, manualised care in insurance-based systems - not that it is ineffective, but that it may not be sufficient for complex trauma, chronic relational patterns, or longstanding attachment wounds.
The backlash isn't really against CBT. It's against reductionism. Against the feeling of being managed rather than met. I've noticed this most starkly when clients describe previous therapy experiences. They rarely complain about cognitive models per se. What they describe is something subtler: "It felt scripted." "It felt like we were working through a checklist." "It helped my panic, but not my shame."

That distinction is important. CBT remains one of the most empirically supported treatments for anxiety disorders and depression. The data is robust. It is cost-effective. It is scalable. In public health terms, it makes sense. But therapy is not only a public health intervention. It is also an intimate human encounter.
And culturally, we are in a moment that prizes authenticity over authority. Transparency over mystique. Therapists who acknowledge their humanity - carefully, ethically - rather than performing neutrality as professionalism.
This shift is visible in training spaces too. Trauma-informed care frameworks, now widely adopted across NHS services and US healthcare systems, emphasise safety, collaboration, empowerment, and awareness of power dynamics. None of that sits comfortably with the old blank slate.
The therapist is no longer just an interpreter of symptoms. They are a regulated nervous system in the room. That doesn't mean boundaries dissolve. It doesn't mean therapy becomes friendship. It means the relational field is no longer treated as secondary to technique.
Psychoanalytic institutes still train clinicians. CBT remains central in public systems. But culturally, the gravitational pull is shifting toward therapies that foreground relationship, embodiment, and co-regulation. The blank slate isn't shattered. It's just harder to believe in.
The Silicon Valley Ingress: AI Therapists and the "Uber-ization" of Care

If the first split in modern psychotherapy is about depth versus symptom management, the second is about something even more structural. Who owns the room? For most of its history, therapy was stubbornly analog. Two chairs. A clock. A door that closed. Then the pandemic forced it online.
Between 2020 and 2022, venture capital poured billions into digital mental health startups. According to CB Insights' State of Digital Health reports, 2021 was a record year for funding in the sector, with mental health companies among the largest recipients. Platforms promised to solve access, scale care, reduce stigma, eliminate waiting lists. And for many people, they did increase access.
In England, NHS Talking Therapies rapidly expanded remote delivery during COVID-19. In the US, telehealth utilization surged across healthcare. A study published in JAMA Network Open in 2022 found tele-health visits for mental health conditions remained substantially higher than pre-pandemic levels even after lockdowns eased.

Remote therapy is not the issue. The business model is. Companies like BetterHelp and Talkspace positioned themselves as marketplaces - matching clients with licensed therapists at subscription rates often lower than private practice fees. But scaling therapy introduces pressures that traditional practice never faced: investor returns, growth targets, churn rates.
In 2023, the US Federal Trade Commission announced a proposed order against BetterHelp for sharing users' sensitive health data with third parties for advertising purposes, including Facebook and Snapchat, despite assurances of privacy.
BetterHelp denied wrongdoing but agreed to pay $7.8 million and to limit future data sharing practices. The case did not argue that therapy itself was ineffective - it raised questions about surveillance capitalism entering the consulting room. The therapy hour became a data stream. And then came AI.
Chatbots such as Woebot and Wysa offer structured, CBT-based conversations available 24/7. Early research suggests some short-term reductions in self-reported depressive symptoms.

A 2017 randomised controlled trial published in JMIR Mental Health found that college students using Woebot reported reduced symptoms of depression over two weeks compared to an information-only control group. That sounds promising. But two weeks is not therapy.
Most AI mental health tools are trained on cognitive-behavioural frameworks precisely because CBT is structured and manualizable. It can be translated into decision trees. It fits the logic of software. Relational depth does not.
Large language models - including generative AI systems - are increasingly being integrated into mental health platforms as "co-pilots" for clinicians or as standalone support tools. Tech companies frame them as scalable solutions to workforce shortages. And workforce shortages are real. The US Health Resources & Services Administration continues to project mental health provider deficits through 2030. Waiting lists in parts of the NHS stretch for months.
The pitch is simple: if humans are scarce, automate. But here is the uncomfortable question. Is therapy primarily information delivery? Or is it an attachment relationship? If it is the former, AI can approximate it. If it is the latter, we are in very different territory.
The risk is not that AI tools exist. The risk is stratification. Affluent clients may continue to access longer-term, relational, trauma-focused therapy. Those with fewer resources may increasingly be routed toward automated or highly standardized care - efficient, scalable, but thinner.

An Uber model of mental health is emerging. Faster matching. Dynamic pricing. Algorithmic triage. The language of disruption has entered psychotherapy. "On-demand." "Optimized." "Frictionless." Words borrowed from transport and food delivery now describe human suffering.
There is genuine good here. Tele-health has increased access for rural communities. Asynchronous messaging platforms offer flexibility for people who cannot attend weekly sessions. Digital tools can complement therapy. But when investor logic meets vulnerability, priorities can shift. The consulting room was once insulated from market forces. It is not anymore.
We are watching therapy become infrastructure. And infrastructure, by design, prioritizes efficiency. The split sharpens here. One future builds tools to reach everyone - quickly, cheaply, at scale. The other insists that some forms of healing cannot be automated without losing something essential.
The question is not whether technology will remain in mental health. It will. The question is whether it becomes an assistant - or the default.
The Fringe: New Psychotherapy Modalities to Watch

Every era of psychotherapy produces its edge. Not the mainstream. Not the institutionally endorsed. The experimental perimeter where clinicians test new maps against old suffering.
Some of these modalities will fade. Some will integrate quietly into existing models. A few may reshape the landscape. Right now, several are hovering at that perimeter.
Deep Brain Reorienting (DBR), developed by psychiatrist Frank Corrigan, is one of them. DBR focuses on early orienting responses in the brainstem - the reflexive micro-movements that occur before conscious emotional processing. The theory suggests that trauma responses are encoded at this subcortical level, and that carefully tracking these micro-sequences can help resolve shock-based trauma.
The evidence base is still emerging. Preliminary studies and clinical reports suggest potential benefit for trauma symptoms, but large-scale randomised controlled trials remain limited. DBR is not currently recommended in NICE guidelines, nor widely embedded in NHS services. It sits, for now, in the realm of promising but developing practice.
Havening Techniques occupy a similar space. Developed by Ronald Ruden, Havening combines elements of exposure therapy with specific forms of touch designed to influence the brain's response to traumatic memory. Proponents argue it can rapidly reduce distress linked to traumatic recall. Critics point out that peer-reviewed evidence is still sparse, and mechanisms remain debated. Systematic, high-quality trials are limited.

"Watch this space" feels appropriate. Because the history of psychotherapy is full of ideas once dismissed that later gained traction - and ideas once celebrated that quietly receded. Then there is eco-therapy.
Unlike DBR or Havening, eco-therapy is less about neurological mechanisms and more about context. It positions mental health within relationship to the natural world - through structured outdoor sessions, conservation work, horticultural therapy, or simply moving therapy outside clinic walls.
This is not purely anecdotal. A growing body of research suggests exposure to green space is associated with reduced stress, improved mood, and lower risk of certain psychiatric conditions. A 2019 study published in Scientific Reports found that people who spent at least 120 minutes per week in nature were significantly more likely to report good health and psychological wellbeing.
In the UK, organizations such as Mind have piloted "ecotherapy" programs, reporting improvements in wellbeing among participants, though much of this data remains observational rather than randomized.
Eco-therapy does not replace trauma work. It does not eliminate depression. But it gestures toward something modern psychotherapy has often minimised: environment.

For decades, therapy largely took place in sealed rooms, abstracted from the ecosystems clients return to after each session. Eco-therapy asks whether healing can occur not only through insight or regulation, but through reconnection - to land, to community, to something beyond the dyad.
What unites these fringe modalities is not a shared technique. It's dissatisfaction with narrow models of change. Some are attempting to go deeper into the nervous system. Others wider into environment and embodiment. All are responding to the same cultural undercurrent: the sense that mental health is not just cognitive error, but systemic strain - biological, relational, ecological.
The danger, of course, is novelty bias. New does not mean effective. The psychotherapy field has seen waves of enthusiasm before. Rigorous research takes time. Replication matters. Mechanism matters. But ignoring the fringe would be equally shortsighted. Because today's experimental edge is often tomorrow's integration.

EMDR was once controversial. Now it is recommended by both the American Psychological Association and NICE for PTSD. Mindfulness-based therapies were once viewed as alternative. Now they are embedded across mainstream services.
We are watching the same early-stage dance again. Careful studies. Conference buzz. Private training cohorts filling quickly. Skeptics raising eyebrows. Early adopters reporting breakthroughs. Watch this space.
The Future of Therapy in a Divided Landscape

Therapy is not collapsing. It is proliferating.
CBT remains the backbone of public provision in the UK, embedded in NHS Talking Therapies and supported by decades of outcome data. Telehealth has expanded access in ways that would have been unthinkable twenty years ago.
AI tools are improving rapidly, and early studies suggest they can deliver structured interventions that reduce mild-to-moderate symptoms in the short term. Trauma research has deepened our understanding of physiology and attachment. Psychedelic-assisted therapies are undergoing regulatory review following promising Phase 3 trial data.
Objectively, this is progress. More options. More reach. More language for suffering. And yet. When I look at where the energy is moving - in trainings, in supervision groups, in the kinds of questions clients are asking - it does not feel like a unified evolution. It feels like divergence.
For clients, this presents a challenge: on the one hand choice has broadened, but on the other, choice has created confusion. Clients still have no clear idea of how modalities approach their inner worlds. Who they work with is still built on practical reasons: recommendations from others, geography, price, experience in presenting issues, and gut feel. I don't see this confusion going away anytime soon.
What I've learned in this exploration is two things:
- How we do therapy is broadening, flourishing even.
- But who gets access to what therapy is becoming a bigger issue.
If public systems - under strain, underfunded, understaffed - increasingly deliver brief, standardized, tech-supported care, while depth-oriented, nervous-system-focused therapies cluster in private practice at premium rates, then therapy does not just split theoretically. It splits socio-economically.
Those with resources may access repair. Those without may receive management. That is not an argument against CBT. Or telehealth. Or AI-assisted tools. Each has evidence behind it. Each has a role. The NHS cannot realistically provide long-term, open-ended trauma therapy to every referral. The US system cannot absorb infinite demand without technological augmentation.
But the question remains. If we accept that trauma is widespread - as the ACE study suggests. If we accept that therapeutic alliance is one of the strongest predictors of outcome. If we accept that some forms of suffering are rooted in attachment injury rather than distorted thought - then what kind of care are we building at scale?
As therapists, we like to believe the room is sacred. Distinct from market forces. Protected from economic logic. It isn't. Investment capital has entered the field. Regulatory frameworks shape modalities. Data dashboards now measure recovery in real time. Algorithms are being trained on therapeutic dialogue.
We are no longer debating which theory of mind is most accurate. We are deciding what kind of system we are willing to create. Will therapy become primarily a public health intervention - efficient, standardised, optimised? Or remain, at its core, a relational encounter that resists automation?
Maybe the future is not either/or. Maybe it is both. But if it is both, then we have to ask something harder than "What works?" We have to ask: Who gets what works? And who decides? That is the real split. Not between modalities. Between models of care.
And we are still, collectively, choosing.