Care for Sale: How Venture Capital Turned the Care of Children and the Mentally Ill Into a Profitable, Quietly Devastating Business
Private equity is reshaping care - from children's homes to mental health services. This piece exposes the moral cost of turning vulnerability into profit and asks: what happens when care is no longer care at all?

A teenage girl sits in a converted Victorian house in Lancashire, one of many children displaced by England's fragmented and profit-driven care system. Her key worker has changed three times in six months.
She's been placed over 100 miles from her family, and the only regular visitor is a social worker drowning in caseloads. What's less visible is the private equity firm that owns the chain of homes she now circulates through - and the £318,000 a year her local authority pays these firms to keep her there. Her trauma has become someone else's investment opportunity.
Across the UK - and increasingly across the globe - a quiet transformation is underway. Care, once the domain of the state, charities, and community, is being financialised. Venture capital, private equity, and multinational holding companies now own significant swathes of residential care, psychiatric services, and mental health clinics. These institutions are no longer judged primarily by their ability to help, heal, or hold the vulnerable - but by their margins, return on investment, and expansion potential.
This isn't just an economic trend. It's a moral collapse. When children in crisis or people experiencing psychosis are viewed through the lens of profitability, society relinquishes its duty of care. We stop asking what people need, and start asking what they can yield.
That's why in this week's Brink, I'm exploring how and why venture capital found its way into caring for our most vulnerable - and how we can find a way out of it.
The Marketisation of Vulnerability

In Britain today, over 80% of children's homes are operated by private companies - many backed by private equity groups whose core mission isn't care, but profit. Their business model is straightforward: acquire a portfolio of homes, standardise operations, cut costs, and extract returns for investors. The result is a care system that increasingly treats children not as individuals with needs but as assets on a balance sheet.
The costs reflect that shift. A single placement in a children's home now averages nearly £320,000 a year, nearly double what it was just five years ago. Much of that cost isn't going toward frontline care - it's being siphoned into debt servicing, dividends, and executive bonuses.
Several local authorities have accused providers of upselling unnecessary support packages to inflate invoices, while homes are often located far from a child's home region - not for therapeutic reasons, but because rural property is cheaper.
In mental health care, a similar transformation is underway. Decades of underfunding, staff shortages, and soaring demand have made the NHS reliant on private providers to plug the gaps. Independent hospitals, some operated by for-profit chains, now account for a growing share of inpatient psychiatric beds.

Many of these facilities are run on thin margins, with stripped-back staffing and high turnover. The pattern echoes what's been seen in the United States, where nearly 15% of psychiatric hospitals are now owned by private equity firms, and care quality has suffered as a result.
Globally, this model is spreading. In Australia, private equity firms now control major disability care providers. In Sweden, the eldercare market is dominated by for-profit chains. In Canada, investment groups have moved into long-term care - with devastating consequences during the COVID-19 pandemic. Across borders, the same logic prevails: when care becomes a commodity, cost control trumps continuity, and margin beats mission.
Why Has This Happened? The Business Case for Human Vulnerability

Venture capital is supposed to be the engine of future-facing innovation - chasing breakthroughs in AI, biotech, and climate solutions. So why is it waist-deep in residential children's homes, mental health clinics, and trauma support services?
Because, unlike space travel or generative algorithms, care has something every investor dreams of: reliable returns.
For private equity and VC funds, the care sector is no longer just a social obligation - it's a market. And not just any market, but a uniquely attractive one: fragmented, under-regulated, structurally essential, and publicly funded. In financial terms, care has become a "defensible asset class" - one that offers consistent demand, low volatility, and high consolidation potential.
I wanted to really understand this in more detail and what I found was five key reasons why money from far flung destinations is pouring into care in your community.
Inelastic, state-backed demand
Even during economic downturns, care doesn't slow down. Children still need to be housed. People still experience mental health crises. Local authorities are legally required to provide services. This creates a rare kind of revenue stability - one backed not by consumer behaviour, but by public obligation. It's no wonder industry analysts refer to the sector as "recession-proof."
Market fragmentation - a goldmine for roll-ups
Most care systems are scattered across hundreds of small providers - many under-resourced, under-capitalised, and overstretched. For private equity, this presents a textbook "roll-up" opportunity: acquire multiple players, consolidate operations, extract efficiencies, and scale into a single, high-valuation platform. It's what happened in eldercare. It's now happening in children's services and behavioural health.
Weak oversight, high opacity
The regulatory structures around ownership and finance in care are often thin. Some providers use complex webs of shell companies to route profits offshore, inflate costs through related-party transactions, or burden operations with debt. According to a Columbia University policy brief, private equity's model thrives on opacity - exploiting gaps in oversight to maximise extraction without direct accountability.
Austerity: the great enabler
A decade of public sector underfunding created a vacuum. Councils, stripped of resources, were forced to outsource more - often to the lowest bidder. Over time, what was once a patchwork of mission-led charities and local authorities became a marketplace dominated by corporate players. With public services in retreat, PE and VC didn't just find space to invest - they found structural dependence.

The "platformisation" of care
The endgame isn't just to run a few homes. It's to build integrated care empires. Investors are increasingly looking to combine residential care, outpatient clinics, therapeutic tech, and logistics under one roof - creating vertical platforms that dominate referral flows and data pipelines. This isn't about care. It's about infrastructure. The same logic that drove VC into cloud storage and delivery apps is now remaking mental health and trauma services.
"Private equity rapidly enlarged its presence in the healthcare sector," notes a recent Stanford Law Review article. "From hospitals and nursing facilities to physician practices and behavioural health... no area is untouched." In Massachusetts alone, private equity's share of health care deals jumped from 32% in 2016 to 64% in 2023.
In short: this wasn't inevitable - it was engineered. Care's moral complexity has been flattened into a business model. And the very qualities that make care sacred - its relationality, its slowness, its unpredictability - are being refactored into operational inefficiencies. What's left is a system designed not to hold people, but to scale them.
Commodification in Practice: How Harm Happens

The damage of financialised care isn't always dramatic. It rarely looks like scandal. More often, it reveals itself in slow erosion - of trust, continuity, dignity. Harm, in this context, is bureaucratised. It appears in missed medications, a support worker who leaves without saying goodbye, a child placed in a home simply because it was the cheapest available bed.
When private equity enters care, the changes are rarely about making things obviously worse - they're about making things more profitable. That often means debt-financed takeovers that saddle care providers with interest payments. Staffing is reduced. Services are streamlined. Specialist roles disappear. Turnover increases. Continuity vanishes. And the people most affected are the least able to complain.
In the US, a major study published in JAMA found that hospitals acquired by private equity saw a 25% rise in hospital-acquired conditions like infections and falls. These aren't abstract metrics - they're avoidable harms experienced by real people, often because corners were cut to protect margins. Central line infections - when bacteria or fungi enter the bloodstream through a central venous catheter (CVC) - for example, rose by 38%, despite fewer central lines being used. That suggests a deterioration not just in care quality but in safety culture.

In residential children's care, similar patterns emerge. Staff, often underpaid and overworked, are stretched thin across multiple placements. Many report being unable to form meaningful relationships with the young people in their care because they don't stay long enough - or aren't allowed to. Some describe pressure to fill beds quickly, regardless of whether the placement is appropriate. Others have raised concerns about staff-to-child ratios that barely meet regulatory minimums.
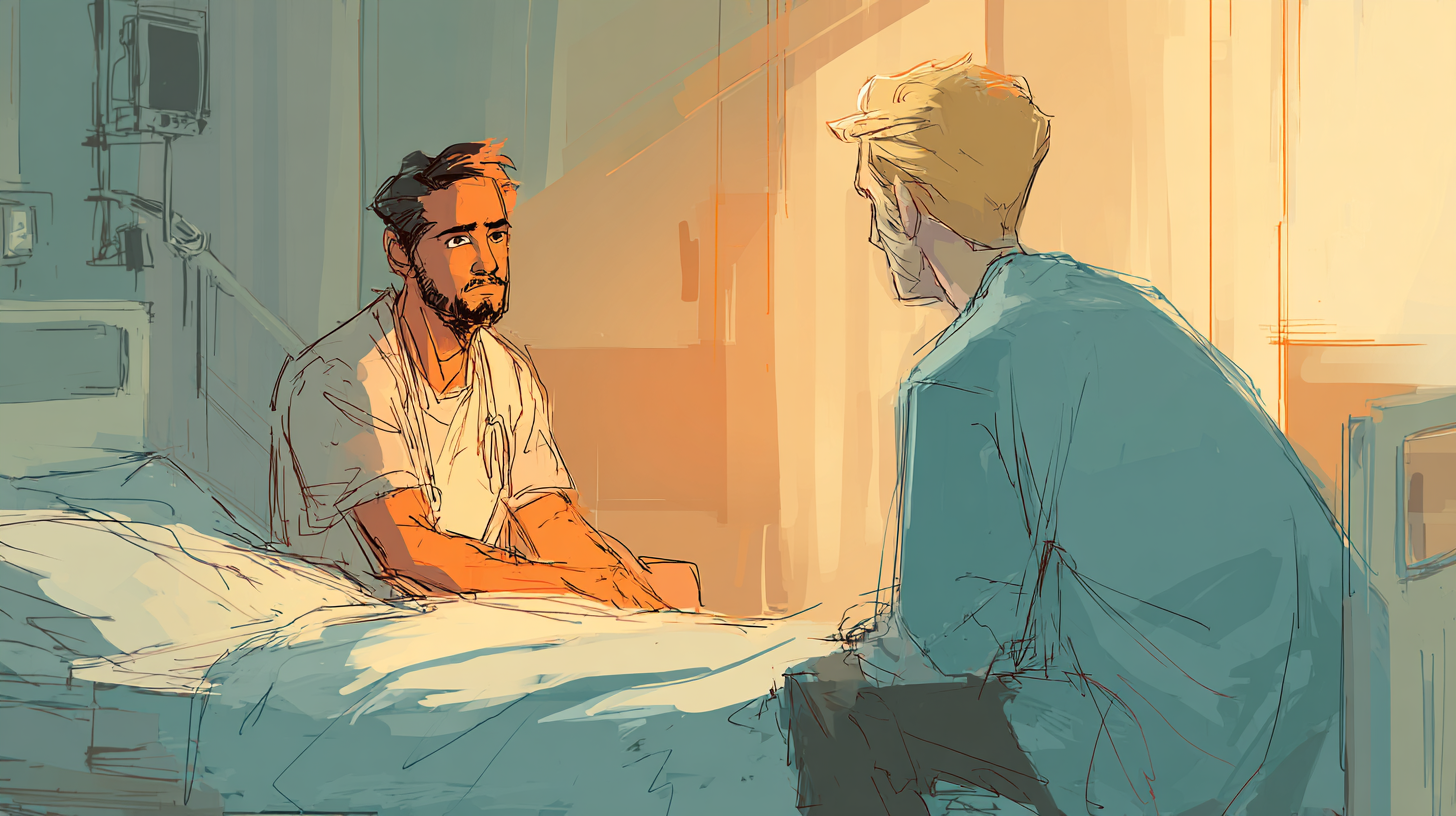
Mental health clinicians, too, speak of moral injury - the distress that comes from knowing what good care looks like, but being unable to provide it. Under investor-owned models, some report being encouraged to increase patient turnover, reduce contact time, or discharge early to keep services moving. The cumulative effect is a system that no longer functions as care, but as logistics: an operation designed not to heal, but to process.
What Gets Lost

In a care system governed by financial logic, the first things to go are the ones you can't quantify. Continuity. Trust. Time. Cultural understanding. Emotional availability. These aren't measured on spreadsheets - but they are the foundation of care that heals.
When children in care are shifted between placements to optimise occupancy rates, they don't just lose a bed. They lose schooling. They lose friendships. They lose a sense of place. Some lose their names - told to adopt new ones to "fit in." Social workers report cases where children have lived in over 20 different placements before turning 18. The system doesn't record that as a failure. It records it as a managed caseload.
For people experiencing mental illness, the losses are similarly quiet. A therapist you've built trust with for six months suddenly disappears because their contract ended. A crisis bed is no longer available because the unit was downsized. Discharge happens too early, because your time is up. The system no longer asks, What do you need? It asks, What can we afford to offer you - and for how long?

For the staff - many of whom came into the field with a deep sense of vocation - the losses are internalised. They speak of burnout, not just from exhaustion, but from grief. Of feeling complicit in harm. Of knowing that something has gone terribly wrong, but being told that "this is just how things work now." They leave the profession not because they want to, but because they can't stand to stay.
None of this fits neatly into a quarterly report. But it accumulates - in missed developmental milestones, in preventable relapses, in care leavers who mistrust every institution they encounter. In a society that no longer recognises the difference between service delivery and human connection.
Skeptics, Caveats, and Counterarguments - and Where They Fail

For all the mounting concerns, defenders of private capital in care often return to a familiar set of arguments - ones that, on the surface, seem pragmatic. But when unpacked, they fail to reckon with the deeper damage unfolding under financialised care systems.
"Capital gives investment and innovation where governments won't."
There's truth in the claim: public systems have been underfunded for years. But the kind of investment that private equity brings is not neutral. It's structurally designed to prioritise extractable value. Investment flows not into long-term trauma care or family-based support, but into services that scale and sell - billing platforms, short-stay crisis beds, diagnostic tech.
This is not innovation in the service of people. It's optimisation in the service of returns.
"Not all private equity-owned facilities perform poorly."
It's true - not every PE-owned care facility is a disaster. Some have stable leadership, committed staff, and acceptable metrics. But metrics often miss what matters most: trust, continuity, cultural safety, relational depth. What's the cost of a child losing a trusted carer? Of a patient discharged too early because the bed is needed?
A system doesn't have to collapse to be doing harm It just has to devalue the things that can't be measured.
"The UK isn't the US - our safeguards are stronger."
In theory, yes. The UK has the NHS, a more centralised regulatory regime, and (ostensibly) stronger professional standards. But austerity has worn those defences thin. Councils are under financial duress. Social workers are overburdened. Ofsted and the CQC have limited reach into complex ownership structures.
The same pressures - fragmentation, outsourcing, underfunding - exist here. The harm just arrives more quietly.

"The problem isn't private equity - it's public disinvestment."
Exactly. This is perhaps the most honest argument - and the most damning. Private equity didn't cause the collapse of public provision; it filled the vacuum. But if the public system had been properly funded, there would have been no space for extractive capital to enter. The very presence of private equity in care is a symptom of a system that abandoned its own mission.
Policy, Resistance, Guardrails, Alternatives
We often talk about care as if it were a fixed thing - either it works, or it doesn't. But the truth is, care is a system we build. And the good news is, systems can be redesigned.
If the financialisation of care was made possible by political choices, policy failures, and institutional neglect - then we can choose differently. We can build guardrails. Reclaim accountability. Invest in care not as a cost, but as a form of social infrastructure. But we have to name what's broken before we can fix it.
Transparency and accountability
We need full public disclosure of who owns what. No more shell companies. No more hidden debt loads or offshore extractions. Care providers - especially those receiving public money - should be required to publish:
- Ownership and corporate structure
- Profit margins
- Debt obligations
- Related-party transactions
- Executive compensation
Public money should not flow to opaque entities extracting wealth from vulnerable lives.
Cap profit, reinvest surplus
Set caps on profit margins for care contracts - particularly in children's services and mental health. Require that any surplus above that line be reinvested into care quality, staff pay, or facility improvement. Care should not be a vehicle for investor windfalls. At minimum, profits should serve the people being cared for.

"Care with dignity" contracts
Move beyond basic service-level agreements. Public authorities should commission care based on trauma-informed, relational, and cultural standards - not just staffing ratios or compliance metrics. Contracts should include:
- Minimum continuity requirements (no arbitrary moves or discharges)
- Community proximity guarantees (no out-of-region placements unless justified)
- Patient or resident voice in care design and feedback
In short: contracts should protect humanity, not just compliance.
Localisation and community anchoring
Encourage smaller, locally rooted providers - non-profits, social enterprises, mutuals - to take up a larger share of care provision. These organisations often have deeper ties to community needs, are less extractive, and more accountable. That means:
- Giving them preferential access in bidding processes
- Providing long-term funding security
- Protecting them from being outbid by multinational chains
Legal and structural reform
Introduce legal limits on consolidation. Ban cross-ownership of placement services and therapeutic providers to avoid monopolised referral loops. Require any care group that crosses a size threshold to be subject to independent review of care outcomes and financial extraction.
If care is a public good, then no single entity should be allowed to own too much of it.
And what can we do?
Not everyone reading this can rewrite care commissioning policy. But everyone can take part in the moral reset this system needs.
- Ask questions. If your loved one is in care, ask who owns the provider. Ask how much is spent on care - and how much is pulled out.
- Support campaigns. Organisations like BASW, Every Child Protected Against Trafficking (ECPAT UK), and openDemocracy are fighting for reform. Join them. Share their work.
- Refuse to look away. The financialisation of care thrives on moral invisibility. On the idea that this is someone else's problem. But it's not. It's a mirror for how we value vulnerability - or don't.
Systems only seem inevitable until we change them. Care can be rebuilt. But only if we treat it like what it is: the moral foundation of a society worth living in.
Naming the Moral Urgency

This isn't about economics. It never was.
It's about the child moved six times in two years because their placement was a line item on a spreadsheet. The man discharged early from a psychiatric unit because turnover targets were tight. The support worker who quit, not out of apathy, but out of heartbreak - because they couldn't bear to keep pretending this was care.
What's happening in children's homes, in psychiatric wards, in supported housing schemes - it isn't accidental. It's structural. It's systemic. It's designed. We have allowed the logic of capital to infiltrate the most intimate corners of human need. We have turned trauma into throughput. Dependency into margin. Vulnerability into yield.

And when we do that - when we look at people who cannot look after themselves and see only cost, efficiency, or opportunity - we lose more than just care. We lose a piece of our collective soul. There is no algorithm for trust. No quarterly metric for belonging. No scalable shortcut to dignity.
So the question is not just how we regulate this system. It's whether we accept it. Whether we believe that care is a relationship, not a transaction. A covenant, not a commodity. And whether we are willing - finally - to act like that belief means something.